HIV and TB Co-Infection Infographic
Learn more about important facts related to HIV and TB Co-Infection
Knowledge centre Description
Learn more about important facts related to HIV and TB Co-Infection

Tuberculosis and HIV co-infection occurs when a person has HIV infection in addition to either latent or active TB disease. Unfortunately, when a person is afflicted with both infections, each disease tends to speed up the progress of the other. Specifically, this means that in addition to the HIV infection speeding up the progression from latent to active TB, the TB bacteria also accelerate the progress of HIV infection.
HIV infections and infections with TB bacteria are two completely different infections. If a person has HIV infection he or she will not get infected with TB bacteria unless there is close contact with someone with active TB, because TB bacteria is spread through small droplets in the air from activities such as talking, coughing, and singing. Similarly if a person has TB, he or she will not get infected with HIV unless he or she carries out an activities, such as sharing drug paraphernalia or having unsafe sex owith someone who already has HIV infection.

When people have a damaged immune system, such as people with HIV who are not receiving antiretrovirals (ARVs), the natural history of TB is significantly altered. While there is often a long latency phase between infection and development of the TB disease that can last years to decades, people with HIV can become ill with active TB disease within weeks to months. It is estimated that the risk of progressing from latent to active TB is between 12 and 20 times greater in people living with HIV than among those who are HIV negative.
HIV positive people with pulmonary TB may have the classic symptoms of TB, which may include fever, loss of appetite, prolonged coughing and coughing up blood, However, HIV positive people may exhibit fewer or less specific symptoms of TB and up to a fifth of those patients may even have normal chest X-rays. This can be attributed to the fact that people living with HIV are more likely to have extrapulmonary TB and this trend appears to be common in countries with a high HIV prevalence, such as South Africa


For adults with HIV/TB co-infection, the patients need to receive both antiretrovirals (ARVs) and TB drugs and the WHO guidelines recommend starting ARVs within the first 8 weeks of starting TB treatment. It is no longer considered necessary to delay the initiation of ARV therapy until TB treatment has been completed. However, the provision of HIV ARV therapy and anti TB drug treatment at the same time involves a number of potential difficulties including: cumulative drug toxicities,
drug – drug interactions, a high pill burden, and the Immune Reconstitution Inflammatory Syndrome (IRIS).
Tuberculosis is the leading cause of death among people living with HIV. In 2019, the mortality estimates were as follows:

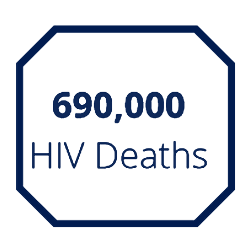
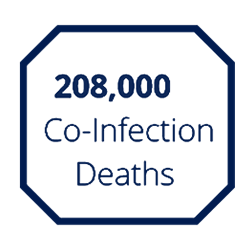
Globally, the mortality for co-infected patients is higher for men than for women in 2019.
97,000 Deaths
Annually for
Men ≥15 Years
76,000 Deaths
Annually for
Women ≥15 Years
19,000 Deaths
Annually for
Boys <14 Years
17,000 Deaths
Annually for
Girls <14 Years
The following illustration summarizes the number of deaths across the WHO regions in 2019.

Africa: 169,000
South East Asia: 20,000
Western Pacific: 6,300
The Americas: 5,900
Europe: 4,200
Eastern Mediterranean: 2,700
Treatment outcome data in 2019 is approximately as follows:
Treatment
Success Rate for
TB Alone
Treatment Success
Rate for
Associated TB
VISIT US AT WWW.MUELLERHEALTHFOUNDATION.ORG AND
FOLLOW US ON TWITTER @MUELLERHEALTH
Source: TB Facts at https://tbfacts.org/tb-hiv/ and
WHO Global TB Report 2020 at https://www.who.int/publications/i/item/9789240013131
Learn more about the 15 most common myths related to tuberculosis.

Learn more about the similarities and differences between tuberculosis and Covid-19.
The figure provides a schematic representation of the major components of the rod-shaped Mycobacterium tuberculosis.

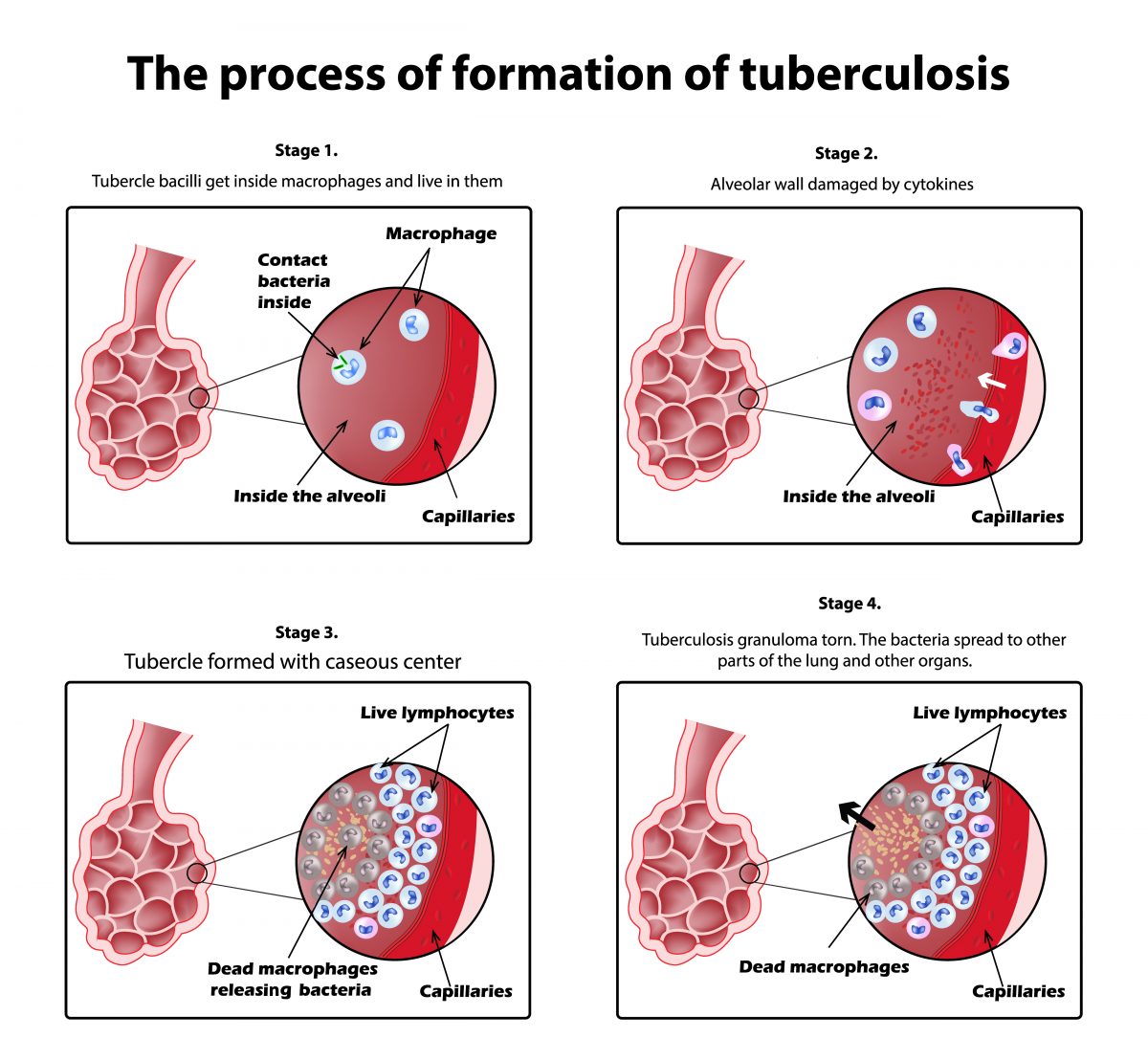
The illustrations provide an overview of the process of tuberculosis formation.
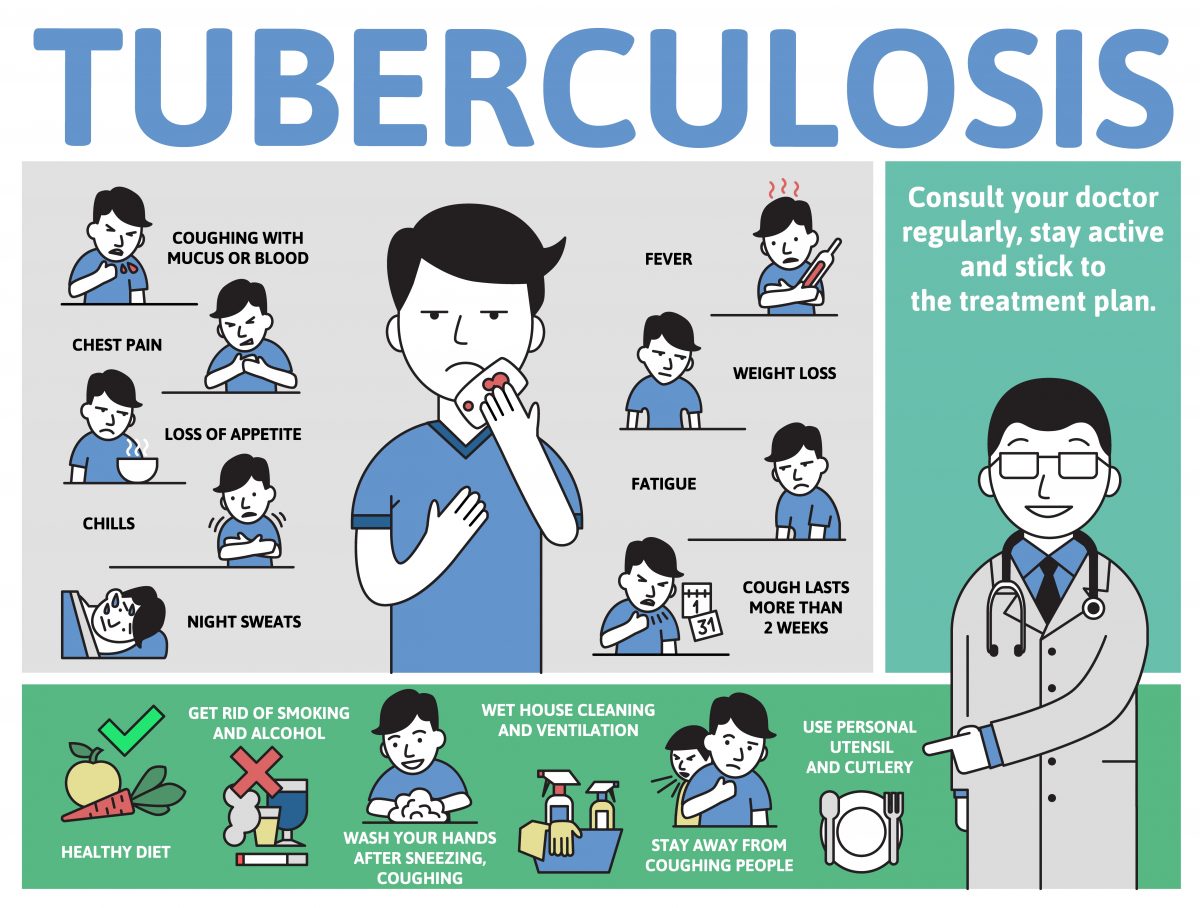
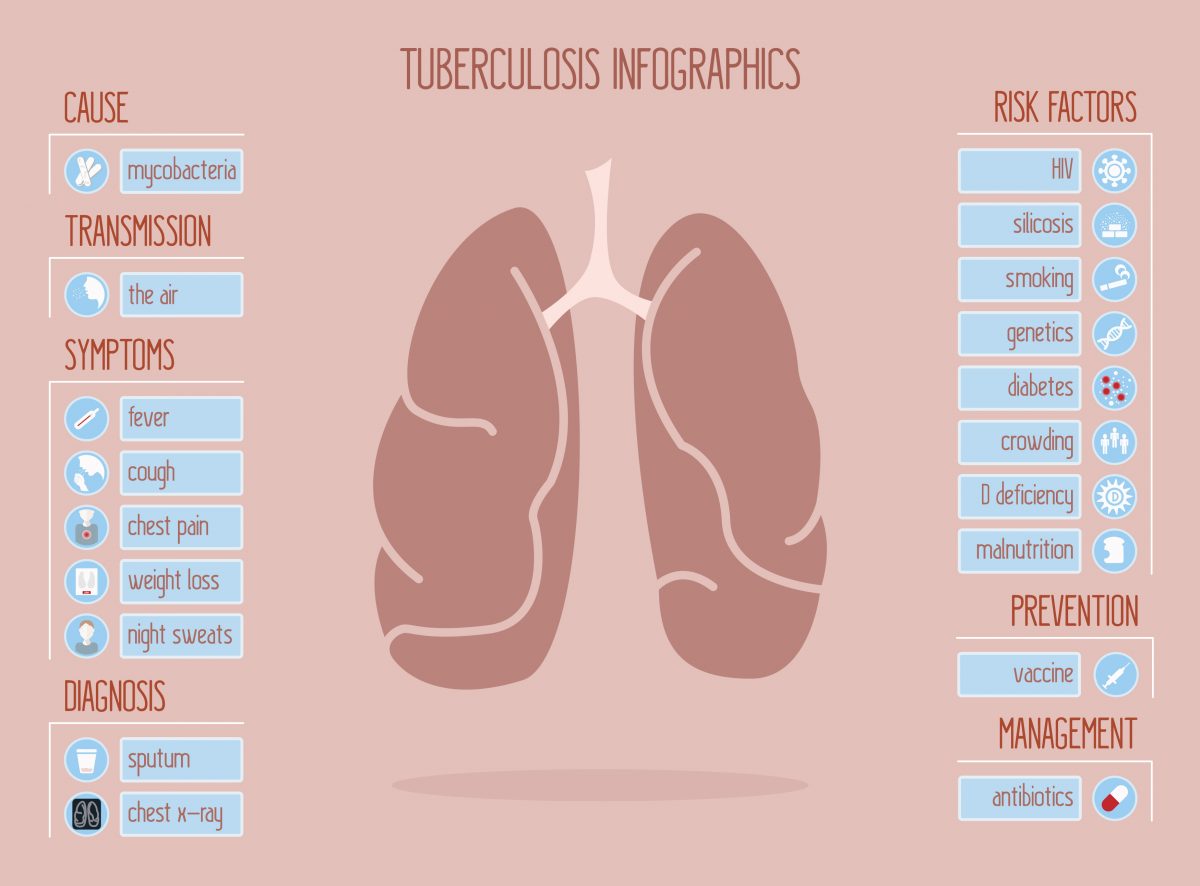
The infographic provides a high-level overview of the cause, transmisson, symptoms, diagnosis, risk factors, prevention, and management of tuberculosis.
The infographic provides an overview of common symptoms associated with active tuberculosis. If you have any concerns or questions about your health, you should always consult with a physician or other health-care professional.